Laboratory Tests and Imaging Modalities for Confirming Scabies Diagnosis
- oluseyi may
- Mar 19, 2024
- 5 min read
Updated: Aug 21, 2024
Every year, millions of people worldwide are afflicted with scabies, a highly infectious skin condition brought on by the Sarcoptes scabiei mite. While recognizing distinctive skin lesions and symptoms is the mainstay of clinical diagnosis, laboratory testing and imaging modalities are also important tools for confirmation of the diagnosis, particularly when symptoms are unusual or equivocal. This article examines the several imaging modalities and laboratory tests that are used to confirm the diagnosis of scabies, highlighting the benefits, drawbacks, and emerging technology in the area.
Diagnostic Laboratory Tests for Scabies
Using a skin scraper and a microscope
By scraping the skin, samples of epidermal tissue are obtained using this conventional approach. The samples are then inspected under a microscope to check for the presence of fecal matter, eggs, or mites. Even though it is regarded as the gold standard for scabies diagnosis, there are some drawbacks, such as its invasiveness and fluctuating sensitivity, especially when there is little mite load or insufficient sample.
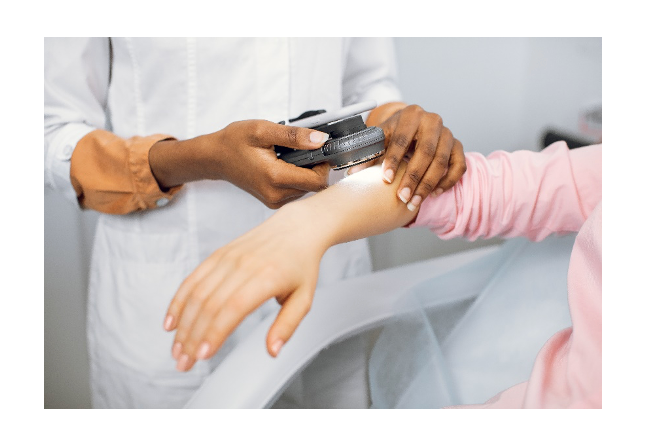
Dermoscopy
Using a portable equipment, dermoscopy allows for greater magnifications of the skin than is possible with the unaided eye. By helping to recognize distinguishing traits like burrows, mites, and eggs, it improves the accuracy of diagnosis. Dermoscopy is a useful diagnostic method for scabies because it is non-invasive and provides real-time imaging. This is particularly true in resource-constrained environments where microscopic investigation may not be easily accessible.
Polymerase Chain Reaction, or PCR
High sensitivity and specificity are provided in the diagnosis of scabies using PCR-based techniques, which amplify and identify certain DNA sequences of the scabies mite. When standard techniques provide conflicting findings or need to confirm a diagnosis in an epidemic that is suspected, this molecular approach comes in handy. PCR tests may be expensive and need certain tools and knowledge, which restricts their use in some situations.
Diagnostic Imaging for Scabies
Dermatoscopy
Dermatoscopy, also known as epiluminescence microscopy, is a portable light-based or non-polarized skin examination device. It helps identify scabies-specific tunnels, mites, and eggs by highlighting skin patterns and structures. Dermatoscopy, a fast, non-invasive outpatient treatment, aids clinical evaluation.
RCM: Confocal Microscopy of Reflectance
RCM is a cutting-edge imaging technology that provides real-time, high-resolution skin cellular imaging. It allows non-invasive observation of mites, eggs, and scabies-related inflammation, improving sensitivity and specificity over standard microscopy. RCM may detect scabies better, but its high cost and requirement for training may limit its adoption.
Sonography
Ultrasonography shows structures beneath the skin using high-frequency sound waves. It is seldom used to diagnose scabies, although studies has shown it may reveal tunnels and fluid accumulations. When other imaging methods are unavailable or inconclusive, ultrasonography may be employed non-invasively.

Skin Biopsy
A skin biopsy may be carried out if the diagnosis of scabies is unclear or if results from other diagnostic techniques are not definitive. A microscopic examination of a tiny sample of skin tissue is performed to look for signs of scabies infestation, such as the presence of eggs, mites, or inflammatory changes. Skin biopsies are intrusive, but they provide histological confirmation of the diagnosis and may help distinguish scabies from other skin disorders that have similar clinical manifestations.
Tests for serology
Specific antibodies against scabies antigens in the blood are detected by serological tests such the indirect immunofluorescence assay (IFA) and enzyme-linked immunosorbent assay (ELISA). Primarily used in research environments, these examinations have the potential to support the diagnosis of scabies, particularly when other diagnostic techniques provide conflicting results. However, because of their inconsistent sensitivity and specificity, serological tests are not often used in clinical practice and have limited therapeutic usefulness.
The Scotch Tape Test
The Scotch tape test involves carefully removing clear adhesive tape that has been applied to skin lesions that may be scabies-infested. After that, the tape is scrutinized under a microscope to check for the presence of feces, eggs, or mites. The Scotch tape test is seldom used in clinical practice and may have lower sensitivity and specificity than skin scraping but is less obtrusive. It may be utilized in resource-constrained contexts when other diagnostic methods are unavailable.
Examining Wood's Lamp
The skin is subjected to UV light during Wood's lamp examination to discover scabies-related fluorescence patterns. Although simple and non-invasive, this method has low diagnostic accuracy and frequently produces false positives. Wood's lamp examination may detect burrows and guide additional scabies diagnostics, but it is not a standalone test.
Cytology
Cytological inquiry involves staining skin scrapings or fluid from skin lesions for microscopic examination. Cytology is not unique to scabies, although it may identify eggs, mites, or inflammatory cells that can confirm the diagnosis. When detecting secondary bacterial infections that complicate scabies infestation or when skin scraping is equivocal, cytological investigation may be very helpful.
IHC, or immunohistochemistry
Using certain antibodies, skin biopsy specimens are stained in immunohistochemistry in order to identify scabies antigens. IHC is mostly used in research settings, but it may also provide further assurance when diagnosing scabies, particularly when histology results are unclear. However, because of its high cost and complicated technical requirements, IHC is not often used in clinical practice.
Molecular Imaging
Novel molecular imaging methods, such positron emission tomography (PET) and fluorescence in situ hybridization (FISH), have the potential to see scabies mites and their metabolic processes in living organisms. Molecular imaging may provide non-invasive, real-time viewing of scabies infestation, enabling early diagnosis and therapy monitoring, even if it is still in the experimental phases. To confirm the clinical value of molecular imaging in the diagnosis and treatment of scabies, further investigation is required.
Digital imaging and telemedicine
With the development of digital imaging and telemedicine, it is now possible to diagnose scabies remotely. Dermatologists don't require in-person consultations to deliver prompt diagnosis and treatment recommendations since they may remotely evaluate high-resolution photos or videos of skin lesions taken by patients or healthcare professionals. Digital imaging and telemedicine may improve access to dermatological treatment even if they cannot replace conventional diagnostic techniques, especially in impoverished regions or during public health crises.
Both machine learning and artificial intelligence (AI)
Scabies and other dermatological disorders are being diagnosed with the use of AI-powered algorithms and machine learning approaches. These algorithms give automated diagnosis recommendations or decision assistance by analyzing clinical pictures, patient histories, and other pertinent data. AI-based diagnostic tools are currently in the early phases of research, but they have the potential to improve patient outcomes in the treatment of scabies, lower healthcare costs, and increase diagnosis accuracy.
Conclusion
Accurate diagnosis is essential for scabies treatment and control. Even while clinical examination is the main diagnosis, laboratory tests and imaging are still needed for confirmation, especially in complicated cases. Clinicians may diagnose scabies using skin scraping, microscopy, PCR, and reflectance confocal microscopy. Technology and research may enhance accessibility and diagnostic accuracy, improving treatment of this common but often overlooked skin illness.









